Medicare Advantage Helpline
Designed an intuitive Medicare Advantage Plan selection experience to help customers find plans that meet their unique healthcare needs.
ROLE
User Experience (UX) Designer
TIMELINE
March 2025 to September 2025
TEAM
1 Creative Director, 2 UI Designers, 1 UX Designer, 2 Product Managers, 2 Project Managers, 1 Researcher, Client Engineering Team, Client Stakeholders
SKILLS
Comparative Analysis, Competitive Analysis, Cross-team Collaboration, User Flows, Figma, Persona, Prototyping, User Testing, Wireframing
Customers are blocked from finding suitable Medicare Advantage plans on their own.
UNDERSTANDING THE PROBLEM
The client, Reliance Medicare Helpline, is a fairly new healthcare brand that aims to connect qualifying customers with Medicare Advantage plans that meet their specific healthcare needs.
The current version (as of March 2025) of the website only allows customers to read the phone number of the Call Center, forcing the customer to navigate away from the site and use their personal phone to contact a representative. Considering customers are unable to search for plans on the website, the clients’ Call Center receives numerous calls from customers looking to find a Medicare Advantage plan that covers their existing doctors, prescriptions, pharmacy, and benefits needs. When speaking with a Call Center representative, customers are unable to access visualizations of their plan options in real time due to the nature of the call being audio only. This frustrating process leads to customers seeking competitors for a more intuitive and hands-on experience in finding a healthcare plan that’s fit for them.
Recognizing the negative implications inflicted on both eager customers and exhausted Call Center representatives, the client asked the Publicis Sapient team to create an experience that will enable customers to find Medicare Advantage plans that meet their unique healthcare needs without needing to contact the Call Center as a first resort.
💭 How might we empower customers to find the right Medicare Advantage plan and reduce the number of calls received by the Call Center?
Understand the experiences customers have on other related websites.
CONDUCTING MARKET RESEARCH
Supported by Jakob’s Law, customers bring their knowledge of how other websites work when visiting the client’s website. Customers will expect Reliance Medicare Helpline to function similarly to the sites they are familiar with. Therefore, I and the UX researcher on the team conducted Comparative Analyses and Competitive Analyses to understand how competitors and other companies create experiences that curate a specific product or service recommendation based on inputs provided by the user.
After research both in-category and out-of-category competitors, I continued to collaborate with the UX Researcher on the team to create a Competitive Experience Comparison Chart. The chart acted as visualization of similar features compared across multiple competitor’s websites to present to clients. Forming this artifact allowed the team to view a summary of the features and experiences customers are likely to expect on the client’s website due to the experiences being prevalent across multiple competitors’ sites.
Identify the features customers will expect to have access to on the client website.
ANALIZING MARKET RESEARCH
Define customer types
UNDERSTANDING THE CUSTOMER
Shopping for a Medicare Advantage healthcare plan is not a one-size-fits-all. Medicare Advantage customers have varying needs, ranging from an individual aging into Medicare with zero major health issues, to an individual who needs coverage for multiple conditions after the discontinuation of a Medicare Advantage plan they’ve had for 10 years.
I collaborated with the Creative Director and UX Researcher on the team to create an artifact that highlights prominent, yet distinct, identifiers of the client’s audience, rooted in data provided by both the internal Publicis Sapient team and the client team.
Developing a clear understanding of the target audience set the foundation for identifying opportunities of problems to solve for the customers, designing with intention, and creating an experience that aligns with the needs and mental models of real customers.
Map the steps customers take
UNDERSTANDING THE CUSTOMER
One main identifier that influences how customers shop is their “Journey Status.” Some Medicare Advantage customers are early in their search for their next healthcare plan. At this stage customers are unsure of their needs and wants. Though, equally likely, other customers are decided in their journey and are ready to purchase a Medicare Advantage plan that meets specific needs in mind.
With the two aspects of Customer Types in mind, I drafted a User Flow to explore the paths customers will take based on their intentions, influenced by their Journey Status. This artifact allowed the team to orient around the steps needed for a customer to provide their healthcare needs, consistent with the steps in competitors’ experiences.
Visualize the path customers take
EXPLORING INITIAL IDEAS
I explored the implementation of the drafted User Flow while keeping in mind the two main Customer Types that influence the steps customers take to select a Medicare Advantage plan:
“Just getting started”
“Decided and ready”
Validate the design with User Testing
TESTING THE DESIGN DIRECTION
I prototyped a mock-up of the “Multi-step” experience for User Testing. The UX Researcher on the team received feedback and gathered insights on both the Multi-step and a Single-step approach created by another designer.
Apply feedback from participants
ITERATING
User Testing results revealed that customers equally preferred the “Multi-step” experience and the “Single-step” experience. Though, more closely, insights revealed:
Customers want to be able to skip health-needs sections that don’t apply to their circumstances.
Customers want to view all of steps upfront.
Customers want to view plan options before narrowing down options and inputting their healthcare needs.
I turned these research insights into action items and applied the findings in the design, allowing the experience to reflect customers’ needs, wants, and expectations.
Integrating key features throughout the experience
CONTINUING EXPLORATIONS
The revised version of the Healthcare Needs Intake flow passed the next round of User Testing. Participants were able to input their needs in a frictionless, fast, and intuitive manner.
Reflecting on the importance of healthcare needs to customers, I proposed the idea of integrating the coverage status of insurance needs in other areas of the website where plan coverage details appear. This suggestion aligns with competitors providing customers the ability to view if specific plans cover healthcare needs, such as the customers’ doctors or prescriptions.
With the intention of prioritizing what’s important to customers and meeting the customers’ expectations of being able to view the healthcare needs status in multiple areas of the site, I explored incorporating “Your Insurance Needs” statuses into Plan Cards, Plan Comparison Pages, and Plan Details Pages.
Considering the limited vertical height of Plan Cards, and the need for internal consistency across the client’s website, I explored with the following constraints in mind:
Simple
Clear
Short (use minimal vertical real-estate)
Ensure usability across the experience
ASSESSING USABILITY HEURISTICS
The next set of designs, which included the integration of coverage statuses across the site, proved to be successful. Overall, participants found the solutions useful, usable, and understandable during the last round of User Testing.
With the proposed direction approved by client stakeholders, given the User Testing results, I took an initiative to assess each screen within the experience, ensuring alignment with the 10 Usability Heuristics.
During my assessment, I uncovered an opportunity to help users diagnose and recover from the issue of having 1 or more of their needs not being covered by a particular plan. I landed on the idea of allowing customers to dive into the experience, uncover which need is not covered, and edit the un-covered need. An example is allowing a customer to change their Brand-name prescription to a Generic prescription.
Implementing this error-recovery functionality allows customers to have the opportunity to receive more Medicare Advantage Plan matches, escaping a “dead-end” of having a need without adequate coverage. Increasing the customers’ chances of receiving a plan-match that covers all of their healthcare needs consequently increases customers’ satisfaction with the client’s website brand. Ensuring error recovery is a customer win, as well as a business win, simultaneously!
Finalize the design
CONCLUDING THE PROCESS
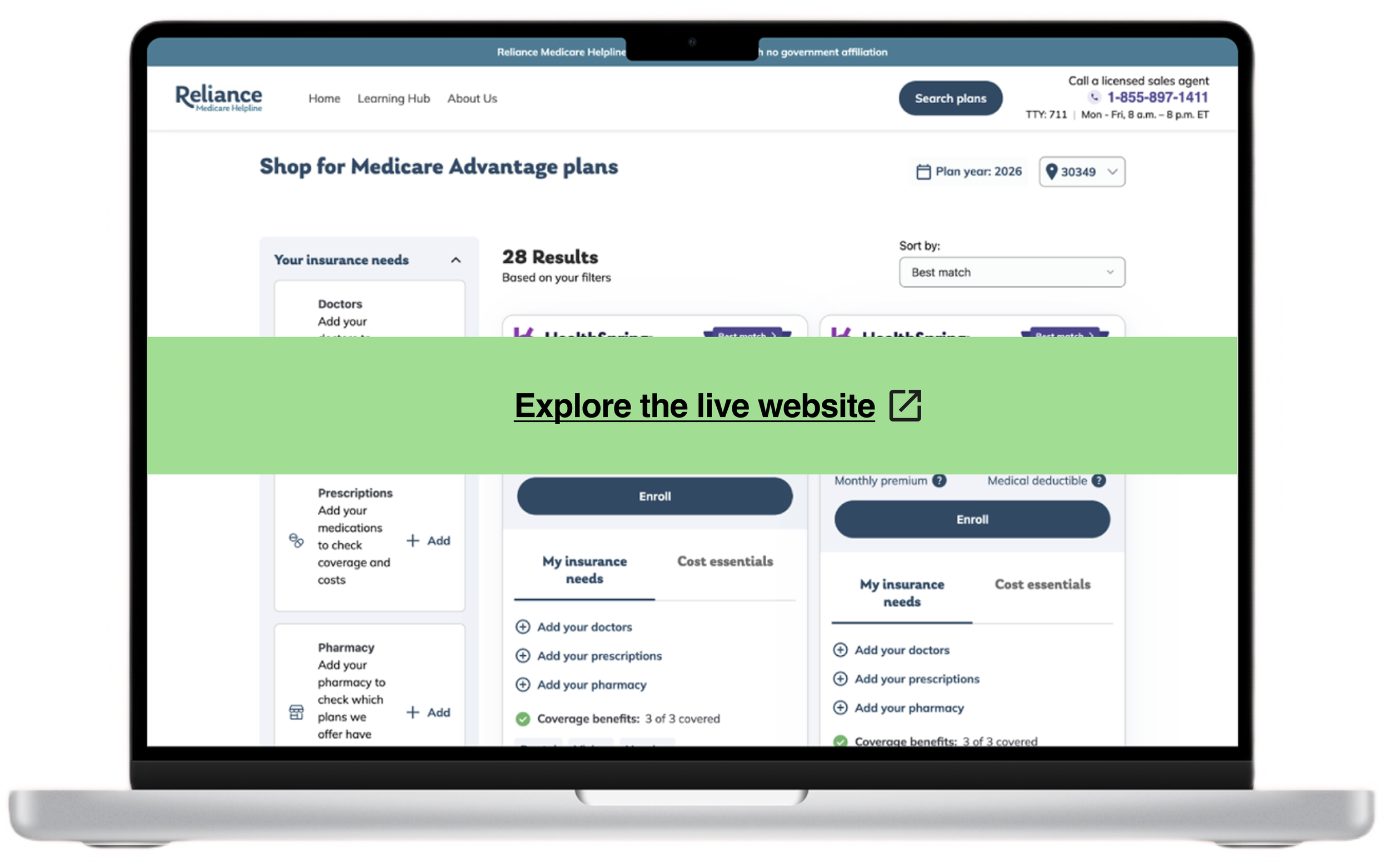
I, along with the rest of the Publicis Sapient team, was able to deliver to the client an experience that enables customers to find Medicare Advantage plans that meet their unique healthcare needs, consequently reducing the need for contacting the client’s Call Center as a first resort.
I successfully designed a user experience (UX) that:
Elevates what’s important to customers - the coverage statuses of their healthcare needs!
Aligns with real world shopping behaviors, validated by User Research.
Reduces friction and dead-ends in the shopping journey by ensuring error recovery.
Increases the likelihood of customers finding 100% plan matches, consequentially increasing customers’ favorability of the client’s brand.
The final designs are live on the Reliance Medicare Helpline website!